The purpose of the Summary of Benefits and Coverage (SBC) is to provide individuals with standard information so they can compare medical plans as they make decisions about which plan to choose.
Effective September 23, 2012, health insurers and self-insured group health plans must provide an Summary of Benefits and Coverage at these times:
- When individuals enroll in coverage for the first time
- At the beginning of each new plan year
- Within seven business days, if an individual requests a copy
This mandate is designed to make health insurance communications more friendly and free of insurance jargon. This part of the law requires that employers provide an “easy-to-understand” Summary of Benefits and Coverage for all employees with private health insurance. This document must summarize the key features of the plan or coverage, such as the:
- Covered benefits
- Cost-sharing provisions
- Coverage limitations and exceptions
Types of plans affected SBCs are required for: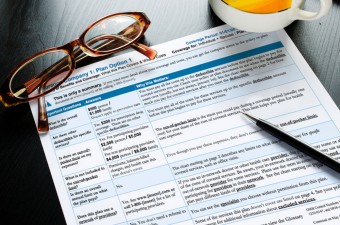
- Individual medical policies
- Insured and self-insured group medical plans, regardless of grandfathered status
Who is responsible for providing the SBC:
- Individual plans: The insurer
- Insured employer plans and HMOs: The insurer and the employer can determine who takes responsibility
- Self-insured plans: The employer
SBCs must be provided during each annual enrollment:
- If an employee must enroll to continue coverage, the SBC must be provided when open enrollment materials are distributed.
- If enrollment materials are not distributed, employees must receive an SBC by the first day they are eligible to enroll.
- For insured plans, if coverage continues automatically for the next year, the SBC must be provided at least 30 days before the beginning of the new plan year. If the policy is not issued by that date, the SBC must be provided within seven business days once the information is available.
- An individual must receive an SBC for the plan in which he or she is enrolled. SBCs for other available plans must be provided on request.
- If any benefit changes are made between the time the SBC is provided and the coverage becomes effective, an updated SBC must be provided. The SBC must be provided within 90 days after an individual enrolls due to a special enrollment event. When an employee requests an SBC, it must be provided within seven business days.
If you have any questions on this matter or need help getting a Summary of Benefits and Coverage for your employees, please contact us and we’ll assist you!
